Brain Patterns, Part 2
How Mitochondria and Inflammation Influence the Brain
At some point, many people notice that their brain no longer feels the way it used to.
Sleep becomes harder to regulate. Focus feels less reliable. Thoughts may feel louder, faster, or harder to organize. For others, the shift shows up as brain fog, emotional reactivity, or a sense that stress now hits harder than it once did.
These changes aren’t random — and they aren’t purely psychological.
The brain is an energy-dependent, immune-sensitive organ. When cellular energy production is strained or inflammatory signaling increases, the brain adapts its output accordingly. Over time, those adaptations become noticeable as changes in sleep, cognition, mood, and stress tolerance.
Two common patterns help explain these experiences: the Wired Brain and the Inflamed Brain. They don’t represent failure or malfunction. They describe how the nervous system responds when metabolic and inflammatory pressure has been building beneath the surface.
Pattern 3: The Wired Brain
(Exhausted… but unable to shut down)
This pattern is familiar to many people, even if they wouldn’t use this name for it.
Common experiences include:
Feeling tired all day but alert or restless at night
Difficulty turning off thoughts
A sense of being “on” even when the body wants rest
Productivity driven by pressure rather than ease
Reliance on caffeine, intensity, or urgency to function
From the outside, the Wired Brain can look like high performance. Internally, it often feels unsustainable.
What’s happening neurologically
The Wired Brain reflects chronic sympathetic nervous system activation. Stress signaling becomes the brain’s default operating mode.
Key neurochemical features often include:
Elevated or mistimed cortisol
Increased norepinephrine
Excess glutamate relative to inhibitory signaling
Reduced parasympathetic tone (lower vagal activity)
But this pattern rarely begins with stress alone.
Why mitochondria matter here
Mitochondria do far more than generate ATP. They help regulate how safe — or threatened — the brain perceives the internal environment to be.
When mitochondrial efficiency declines:
Energy availability becomes less predictable
The brain compensates by increasing stress hormones
Cortisol becomes a backup energy signal
Initially, this works. Over time, it creates a system that cannot easily downshift.
This explains why many people with a Wired Brain report:
Trouble sleeping despite exhaustion
Feeling worse with excessive fasting or overtraining
Short-lived relief from relaxation techniques
The issue isn’t a lack of calming strategies.
It’s a nervous system that no longer trusts its energy supply.
Biomarkers commonly associated with a Wired Brain
Labs are often described as “normal,” but patterns tell a different story. Common findings include:
Flattened or inverted cortisol rhythm
Blood glucose variability or elevated fasting glucose
Low-normal ferritin (reduced oxygen delivery = brain stress)
Low RBC magnesium
Elevated BUN/creatinine ratio (stress + dehydration)
Low heart rate variability (HRV)
Individually subtle. Collectively meaningful.
Why common fitness and nutrition advice can worsen this pattern
Well-intended strategies often amplify the problem:
Excessive high-intensity training → further cortisol elevation
Prolonged fasting → increased stress signaling
Aggressive low-carb approaches → reliance on adrenaline
Forcing relaxation → increased nervous system resistance
The Wired Brain doesn’t need more discipline.
It needs metabolic reassurance and consistency.
General actions that support a Wired Brain
Without protocols or personalization, the most helpful principles include:
Stabilizing blood sugar before adding stressors
Supporting hydration and electrolytes
Repleting magnesium
Favoring rhythmic, moderate movement over intensity
Reinforcing circadian cues (light exposure, meal timing, sleep timing)
Reducing late-day cognitive and sensory load
Calm emerges when the system feels resourced — not forced.
Pattern 4: The Inflamed Brain
(Foggy, reactive, less resilient than before)
The Inflamed Brain is quieter than the Wired Brain — but often more disruptive.
Common experiences include:
Brain fog that fluctuates
Heightened emotional reactivity
Reduced tolerance for stress, noise, or stimulation
A sense of heaviness or pressure in the head
Feeling less cognitively flexible than before
This is not a personality shift.
It’s neuroinflammation.
What’s happening inside the brain
Inflammation alters how neurons communicate.
When inflammatory signaling increases:
Microglia (the brain’s immune cells) become activated
Cytokines influence neurotransmitter signaling
Synaptic efficiency decreases
Cognitive processing slows
The result is a brain that feels less clear, less adaptable, and more reactive.
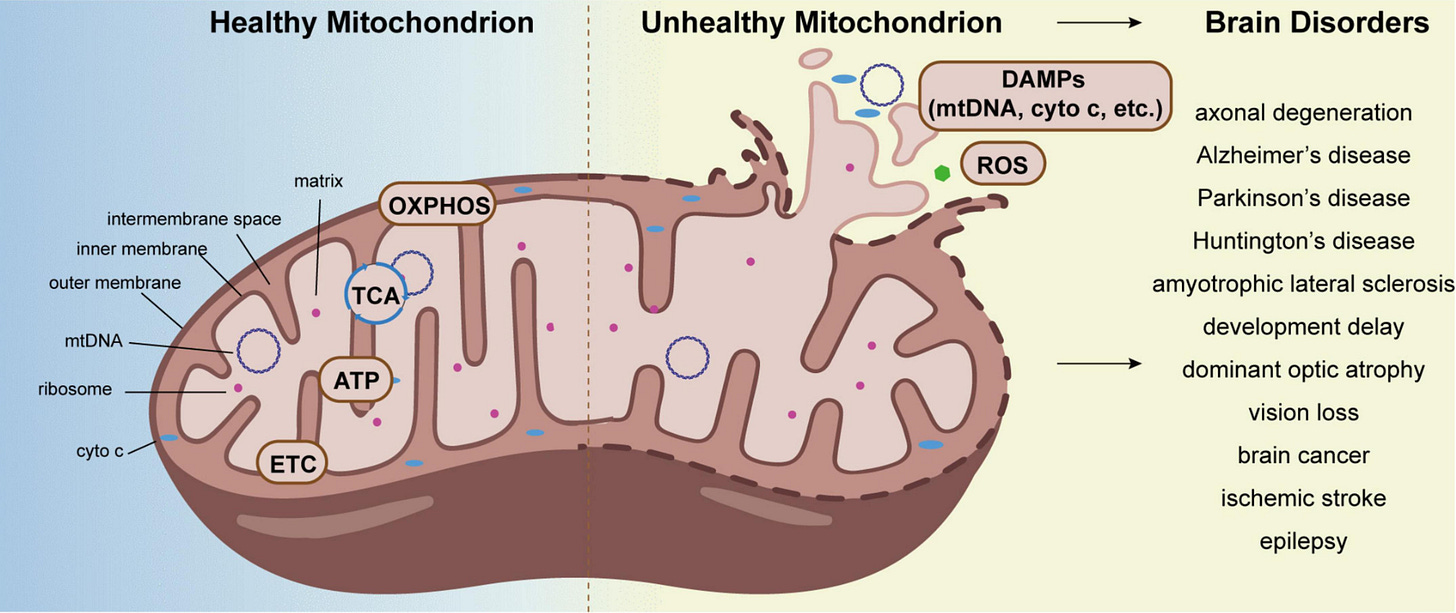
The mitochondria–inflammation feedback loop
Mitochondrial stress and inflammation amplify one another.
When mitochondria are under strain:
Reactive oxygen species increase
Inflammatory signaling rises
Cellular repair capacity decreases
Inflammation then further impairs mitochondrial enzymes, creating a reinforcing loop.
This is why people often say:
“I’m doing anti-inflammatory things, but I still feel inflamed.”
Because inflammation is frequently downstream of energy strain, not separate from it.
Biomarkers commonly associated with an Inflamed Brain
Again, patterns matter more than extremes:
Elevated hs-CRP
High-normal or elevated ferritin
Elevated homocysteine
Increased LDH
Borderline ALT/AST
Markers of gut permeability (when tested)
Low omega-3 index
These markers often live just inside the “acceptable” range — yet align clearly when viewed together.
Why common anti-inflammatory strategies fall short
Inflammation rarely resolves through restriction alone.
Common pitfalls include:
Over-elimination of foods without restoring capacity
Aggressive detoxes that exceed clearance ability
Excessive supplementation adding metabolic burden
Ignoring sleep depth and circadian disruption
Inflammation quiets when the system regains capacity and safety, not just when inputs are removed.
General actions that support an Inflamed Brain
Foundational strategies include:
Reducing inflammatory load without under-fueling
Supporting gut integrity before extreme eliminations
Improving omega-3 intake
Prioritizing sleep depth and regularity
Supporting antioxidant status through whole foods
Lowering cumulative daily stress inputs
Healing requires margin.
Why These Two Patterns Are Often Misidentified
The Wired Brain and the Inflamed Brain are noticeable. They interfere with sleep, mood, focus, and resilience.
As a result, they’re often treated as primary problems — when they’re more accurately adaptive responses to longer-standing metabolic strain.
In many cases, earlier patterns quietly depleted the system first. These patterns simply made the compensation visible.
The brain isn’t failing.
It’s responding.
The Takeaway
If you recognize yourself in either of these patterns, this isn’t a verdict — it’s information.
It tells us:
How your brain has been compensating
Where energy and inflammation intersect
Why willpower-based solutions haven’t worked
When energy production, immune signaling, and nervous system inputs are restored in the right order, the brain doesn’t need to stay wired or inflamed.
Next week, we’ll explore Patterns 5 & 6 — the deeper depletion and disconnection states that often emerge after years of pushing through.
If this article felt uncomfortably specific, that’s not coincidence.
👉 If you want help identifying which pattern is driving your symptoms and where your first domino lives, take the Free Brain Pattern Self-Test.
And if you’d like to be the first to know when enrollment opens for the 2026 NeuroFit Reset, join the waitlist now.
Spots are intentionally limited — because nervous systems don’t heal well in chaos.
Next week, we’ll explore the last 2 patterns- Brain Patterns 5 & 6 — the deeper depletion and disconnection states that often emerge after years of pushing through.
With love & science,
Nikki
References
McEwen, B. S. (1998). Protective and damaging effects of stress mediators. New England Journal of Medicine, 338(3), 171–179. https://doi.org/10.1056/NEJM199801153380307
Picard, M., McEwen, B. S., Epel, E. S., & Sandi, C. (2018). An energetic view of stress: Focus on mitochondria. Cell Metabolism, 28(4), 548–566. https://doi.org/10.1016/j.cmet.2018.07.013
Dantzer, R., O’Connor, J. C., Freund, G. G., Johnson, R. W., & Kelley, K. W. (2008). From inflammation to sickness and depression: When the immune system subjugates the brain. Nature Reviews Neuroscience, 9(1), 46–56. https://doi.org/10.1038/nrn2297
Raison, C. L., Capuron, L., & Miller, A. H. (2013). Cytokines sing the blues: Inflammation and the pathogenesis of depression. Molecular Psychiatry, 18(12), 1248–1257. https://doi.org/10.1038/mp.2013.161
Naviaux, R. K. (2014). Metabolic features of the cell danger response. Mitochondrion, 16, 7–17. https://doi.org/10.1016/j.mito.2013.08.006
Thayer, J. F., & Lane, R. D. (2009). Claude Bernard and the heart–brain connection: Further elaboration of a model of neurovisceral integration. Biological Psychology, 80(2), 246–257. https://doi.org/10.1016/j.biopsycho.2008.08.004
Frontiers in Neuroscience. (2022). Mitochondrial dysfunction and neuroinflammation in neurological disorders. Frontiers in Neuroscience, 16, Article 1075141. https://doi.org/10.3389/fnins.2022.1075141