Brain Patterns, Part 3
The Last Two Patterns — and the Truth That Connects Them All
By now, if you’ve been following along this month, you know this much is true:
Your symptoms aren’t random.
Your struggles aren’t a character flaw.
And your brain isn’t “just like this.”
Over the last few weeks, we’ve been unpacking the six dominant Brain Patterns I see repeatedly in clinical practice — patterns modern medicine often misses, minimizes, or treats in isolation.
Week 1: We named the patterns.
Week 2: We explored the first two foundational drivers.
Week 3: We looked at inflammation and energy collapse — the patterns that quietly derail everything else.
Today, we close the loop.
Because the last two patterns — the ones people chase first — are usually the ones that make the least sense until everything beneath them is understood.
Why These Two Patterns Are So Often Addressed Backwards
If you’ve ever gone looking for answers, chances are you’ve landed here first:
“It must be my hormones.”
“It’s probably my neurotransmitters.”
“If I could just fix this one thing, I’d feel better.”
It makes sense. Hormones and brain chemistry feel tangible. They show up on labs. They have names. They come with supplements, prescriptions, and protocols.
But here’s the part that changes everything:
Hormones and neurotransmitters don’t run the show.
They respond to the terrain they’re operating in.
Which brings us to Brain Pattern #5.
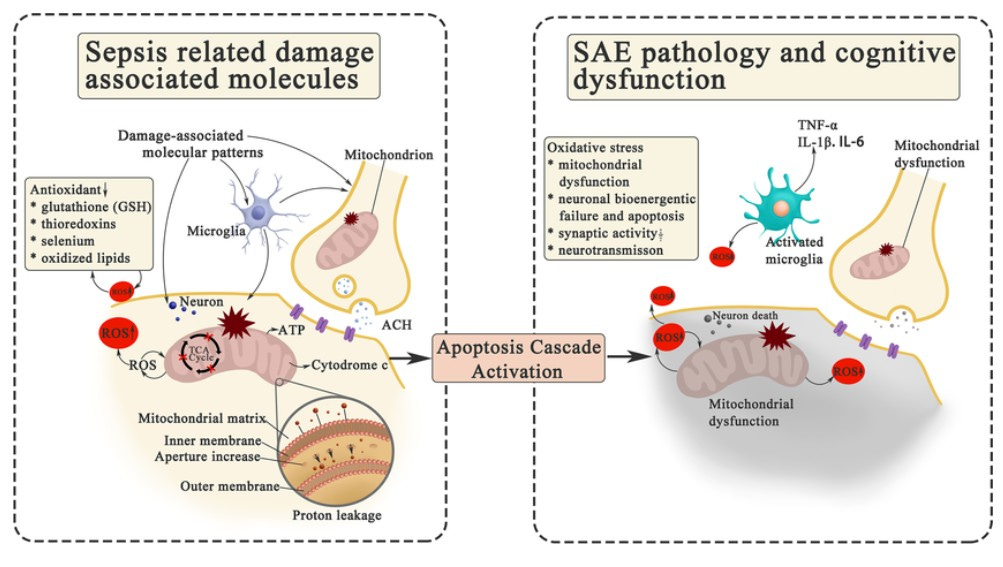
November 2022 Molecular Neurobiology 60(3):1-22
Brain Pattern #5: The Hormonal Brain
(Not a hormone problem — an energy and signaling problem)
This is the pattern that shows up sounding like:
“My mood swings feel random.”
“I don’t recognize myself anymore.”
“My labs are ‘normal,’ but I feel anything but.”
“Every month is a different version of me.”
From the outside, it looks hormonal. And yes — hormones are involved.
But hormones are messengers, not masterminds.
What actually determines how hormones behave is:
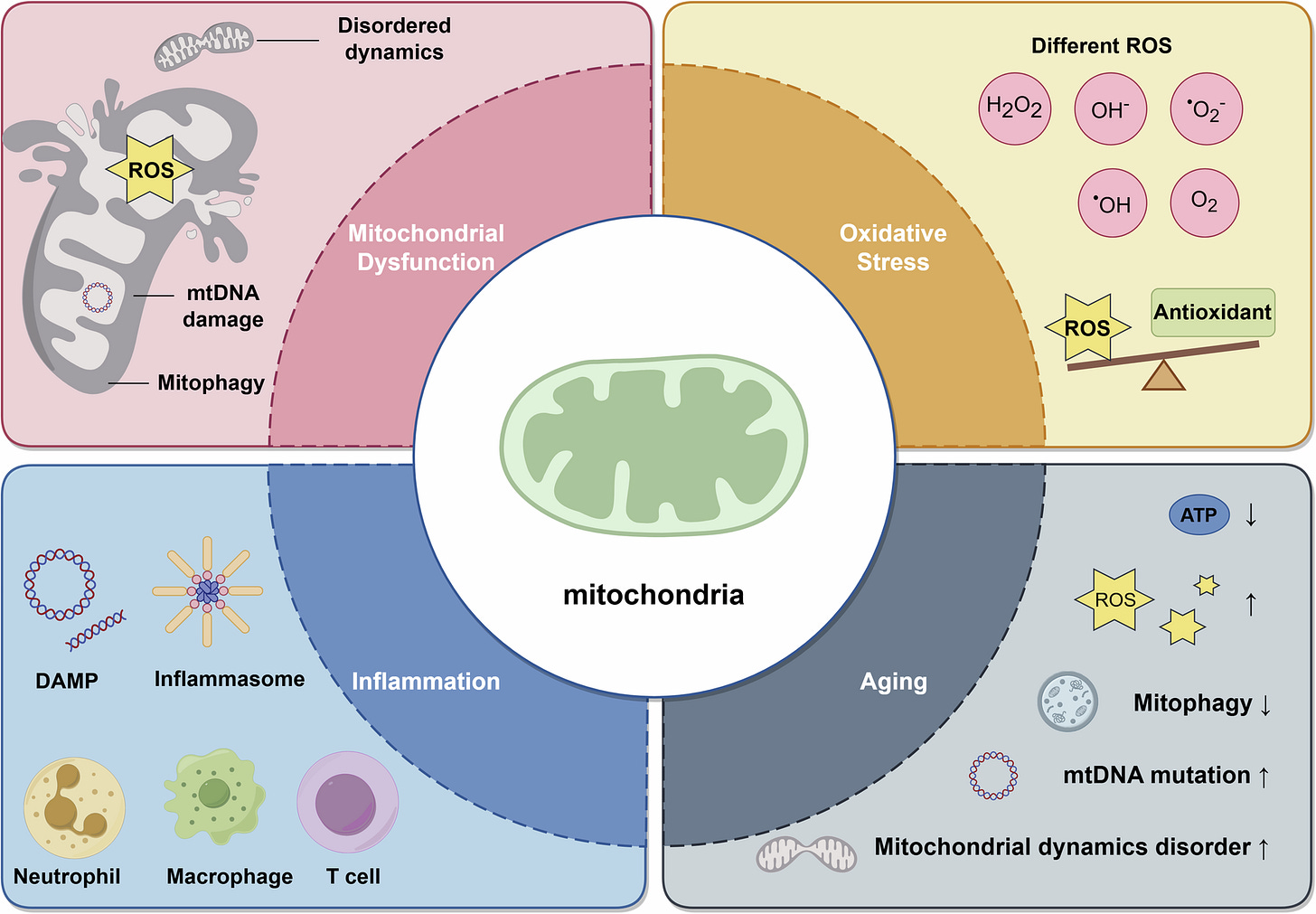
Cellular energy (mitochondria)
Nervous system tone
Inflammation
Blood sugar stability
Detox and clearance capacity
When energy is low, stress is high, and the nervous system never fully downshifts, hormone signaling becomes erratic. Cortisol loses its rhythm. Progesterone stops calming the brain. Estrogen clearance slows. Thyroid signaling becomes inefficient at the cellular level.
So people chase numbers. They tweak doses. They cycle supplements.
And nothing sticks.
Because the real issue isn’t a hormone deficiency — it’s a system under strain.
You don’t “fix” hormones.
You stabilize the system they’re responding to.
Why Hormone Protocols Fail So Often
This is where I want to gently call out what’s happening in the wellness world — especially right now.
We’re throwing hormone protocols at exhausted, inflamed, dysregulated systems and wondering why people feel worse, not better.
December doesn’t help:
More stress
Less sleep
More sugar and alcohol
More emotional load
All of that feeds directly into the nervous system and mitochondria — the very systems hormones depend on to function.
If your hormones have felt like a moving target, that’s not a failure on your part.
It’s a sequencing issue.
Brain Pattern #6: The Neurotransmitter-Depleted Brain
(The most misunderstood pattern of all)
This pattern sounds quieter, but it cuts deeper.
People with this pattern say things like:
“I don’t feel like myself anymore.”
“I know I should care — I just don’t.”
“Motivation is gone.”
“My brain feels flat.”
This is often mislabeled as depression, burnout, or a mindset issue.
It’s none of those.
Neurotransmitters are resource-dependent. They require:
Amino acids
Micronutrients
Enzymatic activity
Adequate ATP (energy)
Low inflammatory interference
Chronic stress drains those resources. Inflammation alters receptor sensitivity. A constantly activated nervous system burns through neurotransmitter precursors faster than they can be rebuilt.
So the brain adapts by down-regulating.
Not because it’s broken — but because it’s protecting itself.
A depleted brain doesn’t need discipline.
It needs biochemical scaffolding.
Why Neurotransmitter Work Is Often Premature
This is where I see people get discouraged the fastest.
They try supplements. Sometimes they try medication. Maybe they feel better briefly… then crash. Or plateau. Or feel like they’re chasing relief that never quite lands.
Here’s why:
If the brain doesn’t have energy, safety, and stability, neurotransmitter support can’t hold.
December makes this especially visible. A depleted brain cannot “push through” the holidays. It shuts down. It withdraws. It flattens affect.
That’s not weakness.
That’s physiology.
The Missing Link That Explains All Six Brain Patterns
This is the thread that ties everything together:
Mitochondria determine how much energy your brain can produce.
The nervous system determines whether your brain feels safe enough to heal.
Inflammation distorts signals between cells.
Hormones and neurotransmitters respond accordingly.
When energy is low and safety is absent, the brain adapts by changing chemistry.
Every. Single. Time.
The Order of Operations (The Map Most People Never Get)
Here’s the hierarchy that changes outcomes:
Restore energy production (mitochondria)
Regulate the nervous system
Reduce inflammation
Support neurotransmitters
Optimize hormones
Address behavior and lifestyle changes
When this order is reversed, people feel like they’re doing everything right — and still failing.
They’re not failing.
They’ve just been handed the wrong map.
What This Means as We Enter a New Year
December is not the time to fix everything.
It’s the time to stop blaming yourself.
It’s the time to recognize that clarity matters more than force.
January doesn’t need a new version of you.
It needs a better sequence.
If you want help identifying which Brain Pattern is driving your symptoms — and where your true starting point is — that’s exactly why I created the Brain Pattern Self Test….for free.
No guessing. No chasing. Just biology, explained clearly.
More to come in the new year — including the 2026 NeuroFit Reset — built intentionally, slowly, and with nervous system safety at the center.
Because healing works best when the brain finally feels supported.
With love & science,
Nikki
References & Further Reading
McEwen, B. S., & Akil, H. (2020). Revisiting the stress concept: Implications for affective disorders. Journal of Neuroscience, 40(1), 12–21.
Picard, M., & McEwen, B. S. (2018). Psychological stress and mitochondria: A conceptual framework. Psychosomatic Medicine, 80(2), 126–140.
Wallace, D. C. (2018). Mitochondrial genetic medicine. Nature Genetics, 50(12), 1642–1649.
Naviaux, R. K. (2014). Metabolic features of the cell danger response. Mitochondrion, 16, 7–17.
Dantzer, R., O’Connor, J. C., Freund, G. G., Johnson, R. W., & Kelley, K. W. (2008). From inflammation to sickness and depression. Nature Reviews Neuroscience, 9(1), 46–56.
Miller, A. H., Maletic, V., & Raison, C. L. (2009). Inflammation and its discontents: The role of cytokines in depression. Biological Psychiatry, 65(9), 732–741.
Sterling, P., & Eyer, J. (1988). Allostasis: A new paradigm to explain arousal pathology. In Handbook of Life Stress, Cognition and Health. Wiley.
Thayer, J. F., & Lane, R. D. (2000). A model of neurovisceral integration in emotion regulation. Journal of Affective Disorders, 61(3), 201–216.
Porges, S. W. (2011). The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-Regulation. Norton.
Yehuda, R., & Seckl, J. (2011). Minireview: Stress-related psychiatric disorders with low cortisol levels. Endocrinology, 152(12), 4496–4503.
Nestler, E. J., Hyman, S. E., & Malenka, R. C. (2009). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience. McGraw-Hill.
Siegel, D. J. (2020). The Developing Mind (3rd ed.). Guilford Press.